
CVR Physician Dr. Pappas Presents Study Findings on Racial Disparity in Vein Treatment
A Center for Vein Restoration physician advances the study of vascular disease with research presented at a European conference.
Peter Pappas, MD, Vascular Surgeon and Director of the Center for Vein Restoration (CVR) Venous and Lymphatic Fellowship Program, offers a continuing medical education (CME) presentation to doctors about pelvic congestion syndrome. Dr. Pappas is the lead physician in CVR’s Union, NJ, and Morristown, NJ, clinic locations.
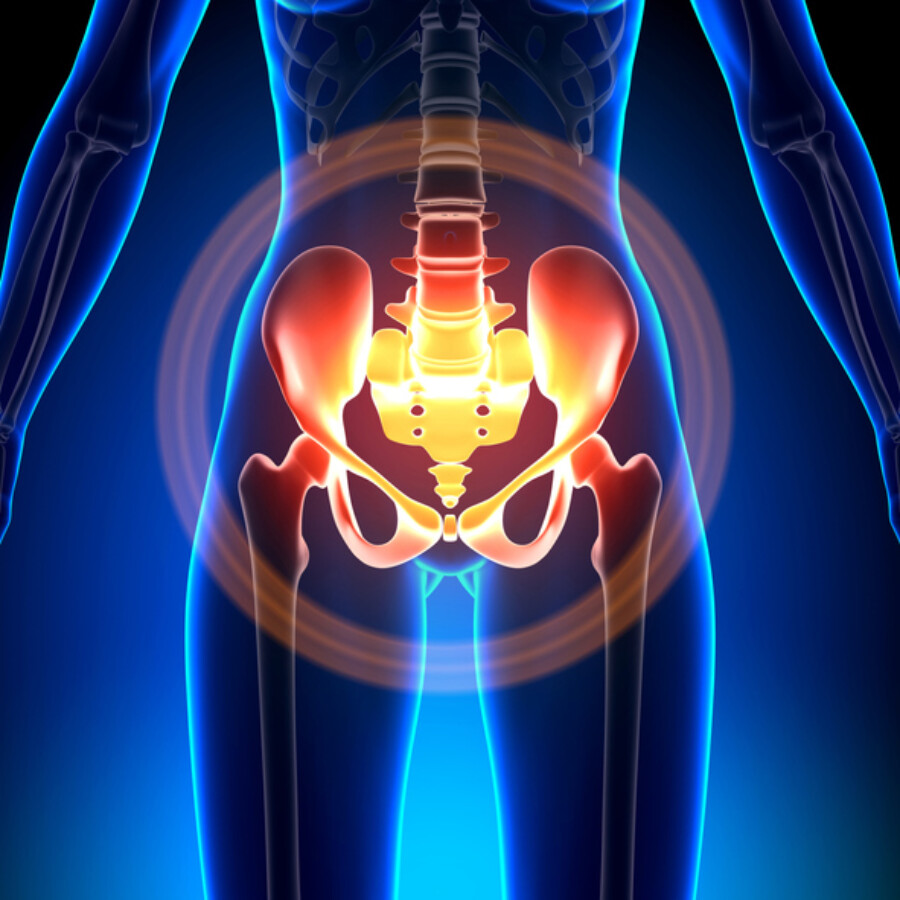
Originally coined during the 1940s, pelvic congestion syndrome is “an old name for a common problem,” according to Dr. Pappas. Caused by dysfunctional veins in the pelvic area, this condition causes chronic, sometimes debilitating pelvic pain. Because the term “pelvic congestion syndrome” doesn’t adequately convey the many causes, signs, and symptoms of the condition, there is a movement underway among professionals in the field to rename it to pelvic venous disorders (PeVD). Dr. Pappas feels that PeVD better describes the multiple pelvic problems that primarily affect women, although the condition can also affect men.
Dr. Pappas explains that the problem with the term “pelvic congestion syndrome” is found in its classic definition, which requires that the patient experience pelvic pain for more than six months (not related to her monthly cycle). The problem with this definition is that many women visit the doctor with a vast array of different symptoms that may or may not be associated with chronic pelvic pain but are still secondary to a pelvic venous disorder.
Dr. Pappas demonstrates just how common chronic pelvic pain is by offering the following statistics:
To emphasize the fact that there is a multitude of causes for chronic pelvic pain, Dr. Pappas presented an overview of other potential causes, which include:
Gynecologic: Including endometriosis, chronic pelvic inflammatory disease, fibroids, ovarian cysts, adhesions, and uterine prolapse.
Urologic: Including interstitial cystitis and recurrent urinary tract infections.
Gastroenterological: Including Irritable bowel syndrome (IBS), Inflammatory bowel disease (IBD), diverticular disease, chronic constipation, and hernia.
Neurologic: Including neuropathic pain and abdominal epilepsy/migraine.
Musculoskeletal: Including pelvic floor myalgia, piriformis syndrome, and psoas inflammation.
Hematological/Oncologic: Including cancer, fibromyalgia, sacroiliac joint pain, and fractured coccyx.
Symptoms include:
Signs include:
In the educational video, Dr. Pappas provides an illustration of the anatomy of the iliac and ovarian veins to demonstrate how reflux occurs. Ovarian reflux is when vein valves in the ovary do not close properly, resulting in backward blood flow, known as “reflux.” Iliac vein reflux is caused by a blockage in the vein that prevents blood from leaving the pelvis in a normal manner
Pelvic vein insufficiency is seen in about 40 percent of women with symptomatic pelvic congestion;
Gynecological perspective: Female patients who come to the Center for Vascular Medicine experiencing symptoms indicative of pelvic congestion first have a gynecological evaluation, including a transvaginal ultrasound to rule out Gynecologic causes of their pelvic pain. Endometriosis and ovarian cysts are the most common gynecologic causes for pelvic pain.
Gastroenterological perspective: Because they are also experiencing pelvic pain, patients often have had an evaluation by a gastroenterologist. These tests can include upper and lower endoscopy, abdominal and pelvic computerized tomography (CT) scan. Dr. Pappas warns that the abdominal and pelvic CT be done with intra-venous contrast, or risk missed interpretation by the radiologist.
Vein disease perspective: Dr. Pappas emphasizes that people experiencing chronic pelvic pain, with or without lower extremity pain and swelling see a vein specialist who can serve as the keystone who pulls together all the test results and interpret them with an eye toward correction of any venous dysfunction. After a thorough history and physical examination, the vein doctor will perform a trans abdominal venous duplex scan to search for evidence of an iliac vein stenosis (narrowing) and ovarian vein reflux. Based upon the history, physical and ultrasound data, the vein specialist will then inform the patient of their treatment options as well as the risks and benefits of each option.
For patients presenting with lower extremity pain, swelling and/or skin changes secondary to varicose veins, a venous duplex ultrasound that evaluates vein function and whether a blood clot is present should also be performed. Patients with persistent pain and swelling after treatment of their lower extremity varicosities should then proceed with a trans-abdominal ultrasound to determine if an iliac vein stenosis is present and possibly contributing to their persistent symptoms.
Dr. Pappas adds that, according to one of his recent peer reviewed publications, over 60 percent of women with pelvic congestion syndrome first present with lower extremity varicosities, pain, swelling and pelvic discomfort. A pelvic vein issue can present with lower extremity pain and swelling without pelvic symptoms. Persistent pain and swelling after addressing lower extremity varicosities are often a sign that a pelvic vein narrowing is present.
Dr. Pappas discusses one of his clinical investigations published in 2018 in the Journal of Vascular Surgery: Venous and Lymphatic Disorders entitled “Iliac vein stenosis is an underdiagnosed cause of pelvic venous insufficiency.” The research studies two hundred and twenty-four women who came to Center for Vascular Medicine for pelvic pain. Their average age was 46 years, and they had experienced an average of over three pregnancies.
The study concluded that 80 percent of women demonstrated significant iliac vein stenosis (narrowing of veins located in the abdomen). And of those women who received ovarian vein embolization and iliac vein stent placement, their symptoms improved dramatically over women who received ovarian vein embolization alone. The exception is women in their twenties who, it was learned, should not be treated with embolization, and stenting as an initial therapy rather, they should have a thorough gynecological examination as their incidence of gynecologic disorders is higher in this age group.
Center for Vein Restoration, the clinical leaders in vein care, is looking for talented, dedicated physicians to join our team. CVR offers a physician-centric model with the freedom to maintain clinical control over medical decisions. If an opportunity to focus strictly on patient care while working with an organization dedicated to improving venous disease outcomes and awareness through philanthropy, innovation, education, and research sounds appealing, visit us at cvrstrongertogether.com.
If you are experiencing chronic pelvic pain, go to the experts who conduct their own research and teach other doctors how to relieve pelvic pain. Call 240-965-3915 to discuss your concern with a patient care coordinator or visit centerforvein.com for more information.